Dr. Ann Kummer spoke to the SLP Impact community and shared some amazing tips for SLPs evaluating velopharyngeal insufficiency (VPI). When we talk about VPI assessments here, we’re not talking about video fluoroscopy or nasopharyngoscopy or any of the fancy medical evaluations. Yes, she and her team do those in the medical setting, but those aren’t available to all of us. We’re talking about VPI assessment techniques that every SLP can do—even school-based SLPs.
Dr. Ann Kummer, Cincinnati Children’s Hospital
First, let me share a bit about Dr. Ann Kummer. She spent her career working at Cincinnati Children’s Hospital, where she led a very large craniofacial program at 12 different locations. Her passion in the field is in the area of cleft palate and craniofacial anomalies. She and her team conduct loads of VPI assessments and have created a process that is very quick and tremendously effective. These are procedures she developed and honed throughout her career in the field, and what I love about them is that they are quick, practical, and packed with information for making diagnostic decisions.
Quick and Accurate VPI Assessment
As SLPs, our field is very broad and for disorders that we see less frequently, we sometimes need to brush up on our skills. For many of us, velopharyngeal insufficiency (VPI) is one of those disorders that we see less often. And most of us do not operate in a medical setting where we are doing video fluoroscopy and nasopharyngoscopy. So, the question is, how do we conduct a VPI assessment for these students when we don’t have access to these technologies? What are we looking for in an evaluation and how can we get the information we need efficiently?
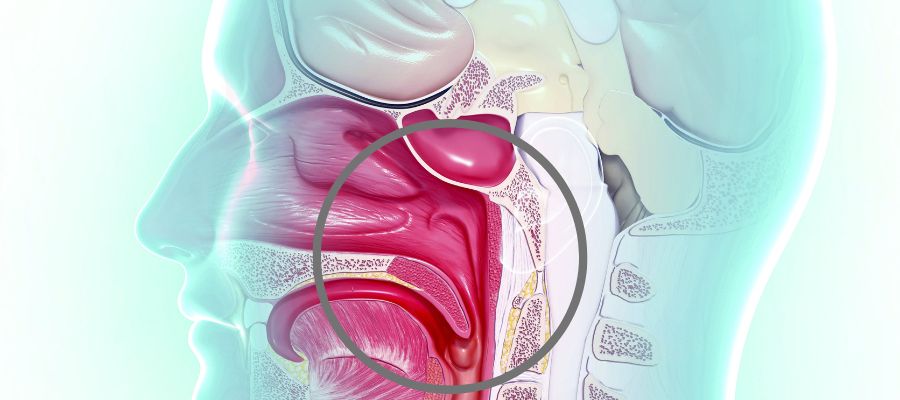
3 Things That Could Go Wrong with The Velopharyngeal Valve
- The first one is abnormal anatomy. That’s what we see when there’s been a history of cleft palate or submucous cleft or post adenoidectomy after tumor removal. And we call that velopharyngeal insufficiency. There is insufficient tissue for closure.
- The next one is abnormal neurophysiology. This occurs when there’s been head trauma or cerebral palsy, or any kind of neural insult or injury. We call this velo pharyngeal incompetence because the velum doesn’t move as well as it should. It might be long enough, but it doesn’t elevate to the level of the hard palate or reach the posterior pharyngeal wall.
- And then there’s abnormal articulation, and we call this velo pharyngeal mis-learning. As an example, if someone learns to produce an NG for an L, you’ll hear, “Njook at the njady” instead of “Look at the lady.” It’s phoneme specific, and it’s because a nasal sound was learned instead of an oral sound.

4 Parts to Evaluation of Speech Resonance and Velopharyngeal Function
Now let’s dive into evaluation of speech resonance and velopharyngeal function. The purpose of the VPI assessment is to make a differential diagnosis. Basically, it’s to determine your recommendations for treatment. That may be surgery, it may be orthodontics, it may be a prosthetic device, speech therapy, or additional referrals. It’s really important that we make the right diagnosis.
So what do we assess? Well, we’re going to assess:
- Speech sound placement
- Nasal emission on consonants
- Resonance on vowels
- Voice
Let’s Start with Speech Sounds
We need to determine if errors are obligatory, compensatory, or developmental.
- Obligatory means that the child’s placement is normal, however, because the velo-pharyngeal valve is open, or maybe because the teeth are in the wrong place, there’s abnormal structure and that’s causing the distortion. Placement is correct but the structural abnormality causes the distortion.
- Compensatory is when the child alters placement in response to the abnormal structure.
- Developmental means the error is typical for the child’s age
Treatment Considerations: For Obligatory and Compensatory errors, the articulation is altered due to the structural abnormality. Therefore, you need to correct the abnormality first.
Next up, Assessment of Nasal Emission
We need to determine if it occurs on all pressure sounds. If nasal emission does occur on all pressure sounds, that means there’s VPI.
We want to consider what it sounds like. If it’s loud, a bubbling sound or friction sound, that would tell you it’s a small opening.
Is the nasal emission phoneme-specific?
Does it occur on one or more of the sibilants?
Now, What About Resonance?
You need to determine the type of resonance, that’s your job.
- Is it normal resonance? In other words, is there a normal balance of oral and nasal resonance? So oral resonance on oral sounds, nasal resonance on nasal sounds.
- Is it hyper nasal? There’s too much sound in the nasal cavity on oral sounds.
- Is it hypo nasal? not enough sound in the nasal cavity on nasal sounds?
- Is it cul-de-sac resonance? Cul-de-sac resonance is when there’s a blockage at the exit of a cavity.
- Is it mixed resonance? There’s hyper nasality on oral sounds and nasal and hypo nasality on nasal sounds.
Are ratings of resonant severity a necessary part of your VPI assessment?
Many people who do cleft palate and VPI assessments feel the need to rate resonant severity. Some use scales of 1 to 5 scale or 1 to 10. Others use severity descriptors such as normal, mild to moderate, moderate, moderate to severe, severe. Another option is simply, “Is it present or absent?” This is what Dr. Kummer proposes we use. Is it present or is it absent? Period. Either there’s hyper nasality or there’s not. That’s much easier to determine, and you’re going be much more consistent in your rating. Severity ratings do not impact our recommendations for either the need for surgery or even the type of surgery. It doesn’t affect our recommendations for the need for speech therapy or the type of speech therapy. If there’s hyper nasality, whether it’s mild, moderate, severe, and it’s due to V P I, which 99% of the time it is, then the only way to correct that is through physical management. And that usually means surgery or prosthetic device if surgery is not possible.
“So, if you have hyper nasality, you need surgical management for correction.”–Dr. Ann Kummer
Voice
Why voice? Because when you see a nasal grimace, there’s also going to be strain in many cases in the vocal folds. There’s also higher incidence of vocal fold nodules in children who have VPI.
We need to assess hoarseness or breathiness because those can be symptoms of vocal nodules, which are common in this population.
We also want to think about pitch. A high pitch can be indicative of a syndrome.
Assessment Tools for VPI Evaluations
Dr. Ann Kummer proposes something controversial. Here’s what she said,
“This is my strong opinion after a very long career, and that is that I think single word articulation tests are not good.”
Why Single Word Articulation Tests Are Not Good for VPI Assessments
- First of all, we don’t communicate with single words, right? So if you have the child produce a single word, that’s going be his best production of the sounds. That is not his typical production, right?
- The second thing is that the speech sound tested can be affected by the phonemic environment. For example, the word “window” was used to test medial D, but it’s proceeded by an N, which is the same placement and a continuant. So the child could even say, “went-oh” and it sounds like there’s a D.
- The other thing is that these tests are expensive, and they’re time consuming. And time is something we need to consider when we’re doing evaluations, because time truly is money. We need to be able to get the information as quickly as possible and have more validity to our tests.
Dr. Kummer’s Assessment Process
We want to test as efficiently as we can but we also want to use methods that are valid and support our diagnostic decisions. So what do I recommend? Well, here are some approaches.
Have the child prolong single sounds to test for hyper nasality.
Use the low vowel like Aaaah, and Eeeee, Believe it or not, there are some kids who have an articulation issue where they raise the back of the tongue on E too high. You wouldn’t know that with an articulation test. Even in connected speech that would be really hard to pick up. You’ll know it if you ask them to prolong a low vowel though.
If you’re concerned about nasal emission, I suggest that you just have the child prolong an [sssssss].It’s a voiceless sound, and that’s important. If it’s voiced, like [zzzzz], you’re going to hear the nasality, the hypernasality, but you’re not going hear the nasal emission. So you always use a voiceless sound that can be prolonged, like [sssssss]. It’s a continuant sound. So you have them go [sssssss] and see when they run out of the air. You can really see that.
Now for a blockage, you use the [mmmmmmmm] because you can tell that the mouth is totally closed. So for hypo-nasality or cul-de-sac resonance concerns, you might want to use an [mmmmmmm], and you’ll quickly see whether they have hypo-nasality or cul-de-sac resonance.
Repetition of Syllables to explore nasal emissions, hyper nasality and articulation errors
Dr. Kummer said that this is one of her favorite tests because she only has to listen to one consonant and one vowel at a time. So you take all the different phonemes that you want to test, and you do it in a repetitive manner. That way it sort of mimics connected speech. It taxes the motor system.
Let’s start with [pa pa pa pa pa, pi pi pi pi pi]. If the child says [ha ha ha ha ha, hi hi hi hi hi], I know he has nasal emission on voiceless sounds.
Next, we do [ba ba ba ba ba, bi bi bi bi bi. If he says [ma ma ma ma ma, mi mi mi mi mi], we know he has nasalization of the [b] sound and hypernasality of the [a].
Next, we try [ka ka ka ka ka, ki ki ki ki ki]. If he says [ta ta ta ta ta, ti ti ti ti ti], that’s an articulation error.
You just take all the different sounds here. If you’re testing hypo nasality, you use nasal sounds.
A Quick VPI Screening
A really quick screening test is having the child count from 60 to 70. You’ve got:
- Connected speech
- Ss
- A triple blend in the medial position, which is great because that really taxes the velopharyngeal mechanism
- A double blend in the final position
- [i] in final position
To test for hypo nasality, include a nasal sound and have them count from 90 to 99 or just repeat 90, 90, 90, 90, 90 or 99, 99, 99, 99. You’ll quickly see whether there is hypo nasality.
Dr. Kummer’s Favorite Test
Take the like phonemes (phonemes that have the same placement with only a difference in voicing) and put them into short sentences. Here are some examples:
- p/b: Popeye plays baseball. Popeye plays in the pool. Buy baby a bib.
- t/d: Take teddy to town. Do it for daddy.
- k/g: Give Kate the cake. Go get a wagon.
Have the child repeat these sentences. If they miss one of them, test what they miss with additional sentences. This takes about 30 seconds to complete this test. It not only tells me what the child’s articulation is in connected speech, which is more realistic, but I could also even do a screening for language problems. So if a child says, “Take teddy town,” Do for daddy,” “Give cake” or “Go get,” or is leaving out any of the other words, I see we need to dive deeper into language during the assessment as well.
Now, what you do is when you report it, is you just report the errors. And you know the truth of the matter is, these tests are faster, easier, and cheaper, but also more valid.

How to Hear VPI
There are a number of approaches people use to hear nasal emissions resulting from VPI.
Seascape
There’s a seascape. You put a tube in the child’s nose. There’s a little styrofoam stopper. When you say, “pop, pop, pop,” it shouldn’t move. If there’s nasal emission, the styrofoam thing inside moves. Here’s the problem, you cannot clean it. There’s no way to sanitize it. So it’s a germ magnet. If you want to use this, you’d have to buy a new one for every person you tested, and they aren’t inexpensive!
Stethoscope
You could use a stethoscope. A stethoscope is great because what you can do is you can put the drum near the nose, or even better, you can take the drum off and put the whole tube in the nose and you listen. What you’re doing is sending sound through this tube, and that amplifies the sound. The problem with the stethoscope though is that you have to clean it.
Bendy Straw
A third and better option is using a straw. Put the tip of the straw in the nose. A bending straw is always best. The short end goes in the child’s nose, you move the longer end toward your ear.
Ask the child to say, “pa pa pa pa pa” If you have a normal velopharyngeal valve, you should hear nothing on oral sounds. Zero. If you hear something, you’ve got a problem. If you have nasal emission, you’ll hear it very loudly through the straw. If you have hyper nasality, you’ll hear it through the straw. This is an easy, quick way to identify VPI.
Now, On to the Intraoral Examination
Dr. Kummer shared two quick tips for the intraoral examination. First, it can be tricky to get a nice view inside the child’s mouth to see if there is a fistula or submucous cleft. Grab a dental mirror, shine your light on the mirror to make the light pop up and illuminate the roof of the mouth.
Once you can see in the child’s mouth, our go-to is to have the child say “ah” but then you need a tongue blade because saying “ah” makes the back of the tongue go up and then we can’t see what we need to see. Dr. Kummer suggests asking the child to try and touch the his chin with his tongue. Then you can see the entire back of the mouth. You can even see the epiglottis pop up in some cases.
Easy, Effective and Fast ways to Evaluate VPI in any Setting
So there you have it. Some great, effective, easy, quick, and cost-effective evaluation techniques to determine the presence or absence of VPI. Thank you, Dr. Kummer, for making this easy for us!